Being told you have to undergo an endoscopic procedure can be frightening for a lot of individuals. You may fear having a complication, experiencing major discomfort, or even having an unsuccessful outcome. These fears are the reasons why appropriate behavior must be observed in and out of the endoscopy room. The endoscopy team must realize and understand how major the procedure may seem to the patient and they must respect and sympathize with them throughout the entire process.
Preparing for an Endoscopy
Preparation is an essential part of this process for both the patient and the endoscopy room. Patients must be prepared both mentally and physically and it’s in the hands of the physician to make sure this happens. The physician is the chief of the procedure and holds a heavy responsibility regarding patient safety and convenience.
Before the procedure, the physician should review all details and risks with the patient as well as obtain informed consent and answer any questions they may have. These procedures are pretty routine, but sometimes accessory procedures emerge. The physician should go over this with the team so they are prepared since it might require additional equipment that isn’t routinely used. It is also pertinent that the physician reviews this possibility with the patient. Discussing the technique and the sensations that they may experience can be really helpful. This allows the patient to feel assured that the physician understands their uneasiness or fears.
What Happens During an Endoscopy?
The patient should always have their complete attention, which means pager beepers are to be silenced and under no circumstances should the staff answer phone calls in the endoscopy room. The endoscopy assistant should primarily focus on the patient’s general comfortability levels and monitor vital signs. Some common sources of patient discomfort may include pinching from the endoscope mouthpiece, or an itching sensation of the nose or mouth. The assistant should constantly be aware of these and help prevent discomfort whenever possible.
A major concern during the procedure is the patient’s comfort relative to body position and environmental awareness. Remember that the patient is still able to hear, so conversations should remain focused on the patient or the procedure. Avoid whispering that may lead to laughing. This may cause the patient to think their topic of conversation is related to his or her condition, which could likely cause stress or panic, which would be troublesome for both the patient and the endoscopy team. Along with appropriate conversation, it’s important for the physician to periodically reassure the patient of the progress being made so that they remain calm and confident in their mental state.
Some patients want the option to observe the video monitor as they conduct the procedure, but permission is needed by the physician. If they request to watch, the physician must make a choice whether or not to grant them permission based on the personality of the patient, the type of procedure and the risks involved. If the physician allows them to observe, he or she must accept full responsibility if the patient acts out or experiences any psychological episodes. However, visual encounter with any scopes or other equipment should be avoided. This could cause distress, much like what a child experiences when they see the doctor holding a flu shot and the needle is visible.
What Happens After an Endoscopy?
Post procedure, the physician should give patients the courtesy of a post-procedural appointment, as well as letting them know they can contact them by telephone if they have any questions or concerns. Behavior is a huge factor in the surgery process, so adhering to these criteria will help the procedure run smoothly.
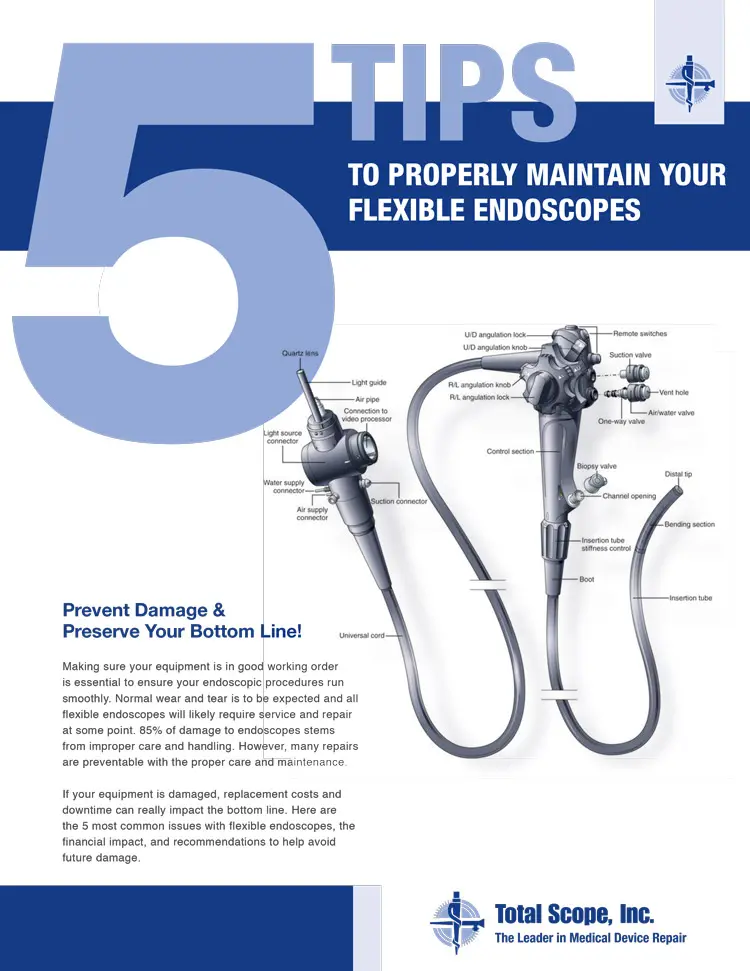
The room used for the procedure is always thoroughly cleaned, along with the endoscope and other equipment. For some tips on how to maintain your endoscopes & troubleshoot problems, visit our preventative maintenance guide.
 FREE SHIPPING Anywhere in the Country for Repairs
FREE SHIPPING Anywhere in the Country for Repairs